Why Mammography is NOT an Effective Breast Cancer Screen
Dr. Mercola
The most devastating loss of life from breast cancer occurs between the ages of 30 to 50. Fortunately, you have more options available to you today to help detect breast cancer than in the past decades.
Unfortunately, education and awareness of these options and their effectiveness in detecting breast cancer at different stages in life are woefully deficient.
Beyond Mammography
In the first part of the in-depth article linked below, Beyond Mammography, Dr. Len Saputo explores the latest findings on the effectiveness and shortcomings of various detection methods used by the mainstream medical community, including mammography, clinical breast exams, ultrasound, and to a lesser extent, magnetic resonance imaging (MRIs) and PET scans.
The second part goes beyond mammography, exploring a highly advanced but much maligned detection tool for breast cancer -- breast thermography.
Breast thermography, which involves using a heat-sensing scanner to detect variations in the temperature of breast tissue, has been around since the 1960s. However, early infrared scanners were not very sensitive, and were insufficiently tested before being put into clinical practice, resulting in misdiagnosed cases.
Modern-day breast thermography boasts vastly improved technology and more extensive scientific clinical research.
In fact, the article references data from major peer review journals and research on more than 300,000 women who have been tested using the technology. Combined with the successes in detecting breast cancer with greater accuracy than other methods, the technology is slowly gaining ground among more progressive practitioners.
About the Author
Dr. Len Saputo, MD, is a graduate of Duke University Medical School, and is the Founder and Director of the Health Medicine Forum, which has hosted and moderated over 350 events. He's also the Co-founder and Medical Director of the Health Medicine Institute and Health Medicine Center, and runs a private practice in Internal Medicine and Health Medicine.
|
What You Should Know About UVA and UVB Rays Ultraviolet light from the sun comes in two main wavelengths – UVA and UVB. It’s important for you to understand the difference between them, and your risk factors from each. |
| Find Out More |
| Dr. Mercola's Comments: | |
|
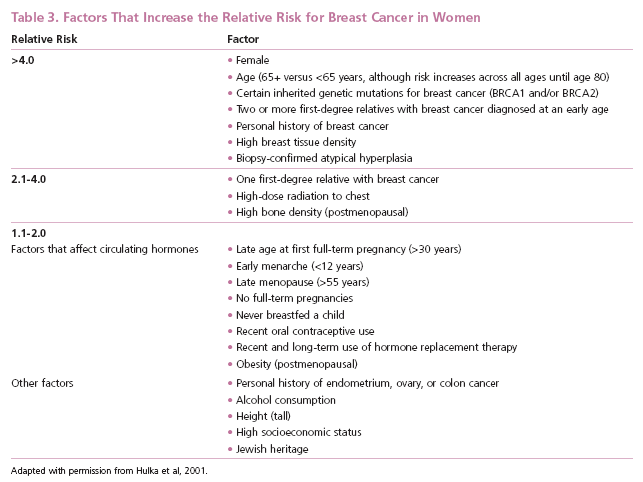
Breast cancer is the second most deadly form of cancer for women in the U.S. Only lung cancer claims more women’s lives than breast cancer. According to Cancer.org’s latest report, Breast Cancer Facts & Figures 2007-2008, 2007 ushered in more than 178,000 new cases of invasive breast cancer, and more than 40,000 women died from the disease. But men are by no means immune to breast cancer. Just over 2,000 men were diagnosed with breast cancer in 2007, and approximately 450 men died. Since routine screening for men is next to nonexistent, men are more likely to be diagnosed with advanced disease, and therefore have poorer chances for survival. Unfortunately, conventional medicine is stubbornly holding on to outmoded ideas of cancer detection and treatment, no matter how ineffective it’s been proven to be. Mammography is a perfect example of this stubborn head-in-the-sand approach to cancer screening. Education and awareness of better, less risky and more effective options for detecting breast cancer are woefully deficient, but they do exist, and it is my hope you will take the time to review this important information, whether you’re a man or a woman, and forward it widely to your family and friends. The Case Against Mammography Health officials recommend that all women over 40 get a mammogram every one to two years, yet there is no solid evidence that mammograms save lives, and the benefits of mammograms are controversial at best. Meanwhile, the health hazards of mammography have been well established. John Gofman, M.D., Ph.D. – a nuclear physicist and a medical doctor, and one of the leading experts in the world on the dangers of radiation – presents compelling evidence in his book, Radiation from Medical Procedures in the Pathogenesis of Cancer and Ischemic Heart Disease, that over 50 percent of the death-rate from cancer is in fact induced by x-rays. Now consider the fact that the routine practice of taking four films of each breast annually results in approximately 1 rad (radiation absorbed dose) exposure, which is about 1,000 times greater than that from a chest x-ray. Even the American Cancer Society lists high-dose radiation to the chest as a medium to high risk factor for developing cancer.
How Mammography Increases Your Cancer Risk X-rays and other classes of ionizing radiation have been, for decades, a proven cause of virtually all types of biological mutations. When such mutations are not cell-lethal, they endure and accumulate with each additional exposure to x-rays or other ionizing radiation. X-rays are also an established cause of genomic instability, often a characteristic of the most aggressive cancers. Additionally, radiation risks are about four times greater for the 1 to 2 percent of women who are silent carriers of the A-T (ataxia-telangiectasia) gene, which by some estimates accounts for up to 20 percent of all breast cancers diagnosed annually. When everything is taken into account, reducing exposure to medical radiation such as unnecessary mammograms would actually likely reduce mortality rates. The practice of screening mammography itself poses significant and cumulative risks of breast cancer, especially for premenopausal women. Making matters even worse, false positive diagnoses are very common – as high as 89 percent – leading many women to be unnecessarily and harmfully treated by mastectomy, more radiation, or chemotherapy. There are instances where mammography may be warranted. But the fact remains that there are other technologies that are proven to be more effective, less expensive, and completely harmless, that can save far more lives. Now, imagine being able to look inside yourself and be able to get as much as 10 years warning that something is about to develop, giving you ample time to PREVENT the cancer from forming in the first place by taking the appropriate lifestyle changes that can radically change your health. That technology already exists, and has been available since the 1960s. Thermographic Breast Screening – A Safer, More Effective Alternative Most physicians continue to recommend mammograms for fear of being sued by a woman who develops breast cancer after he did not advise her to get one. But I encourage you to think for yourself and consider safer, more effective alternatives to mammograms.
The option for breast screening that I most highly recommend is called thermographic breast screening. Thermographic screening is brilliantly simple. It measures the radiation of infrared heat from your body and translates this information into anatomical images. Your normal blood circulation is under the control of your autonomic nervous system, which governs your body functions.
Thermography uses no mechanical pressure or ionizing radiation, and can detect signs of breast cancer as much as 10 years earlier than either mammography or a physical exam! Whereas mammography cannot detect a tumor until after it has been growing for years and reaches a certain size, thermography is able to detect the possibility of breast cancer much earlier. It can even detect the potential for cancer before any tumors have formed because it can image the early stages of angiogenesis -- the formation of a direct supply of blood to cancer cells, which is a necessary step before they can grow into tumors of size. More men’s lives could also be spared from the disease as mammography is not frequently used on men, which leads to most men with breast cancer being diagnosed at a very late stage. Other Risk Factors Commonly Ignored and How You Can Avoid Them Breast density and high levels of circulating sex hormones are two commonly known risk factors for breast cancer in post menopausal women. A 2007 study published in the Journal of the National Cancer Institute confirmed that although the two factors commonly occur together, they are also independent risk factors. They found that (after controlling for other factors) when breast density was not considered, women with high amounts of circulating sex hormones had twice the risk of developing breast cancer as those with low amounts. And, women in the highest one-quarter in density had four times the risk of those in the lowest quarter, without considering levels of sex hormones. Women with both the highest hormones and densest breasts had up to six times the risk. The authors of the study highlighted the importance of screening and, perhaps most importantly, maintaining a healthy, lower weight to help keep hormone levels lower. In fact, excess body weight and obesity plays a significant role in a number of cancer deaths, admits the American Cancer Society. But there are other factors that will increase your risk of breast cancer that few ever bother to mention. For example, a 2001 study published in the British Journal of Cancer discovered that women with breast cancer are twice as likely to have a fault in the gene required to make use of vitamin D. The research suggested that women with genetic variations (polymorphisms) of the vitamin D receptor gene may be less able to benefit from this protective effect. Experts already believe vitamin D protects against breast cancer and in some forms may even be used to shrink existing tumors. According to recent research from Stanford University, optimal amounts of sunlight exposure may reduce your risk of advanced breast cancer by as much as 50 percent. I believe sunlight is so imperative for disease prevention and for your overall health I even wrote a book on the topic called Dark Deception, which is due out shortly.
Your omega-3 to omega-6 ratio can also play a significant role. One study, published in the International Journal of Cancer in 2002, discovered that omega-3 fatty acids did indeed have a protective effect against breast cancer. This supports the imperative balance of your omega-3 to omega-6 ratio as being important in the development of breast cancer in the first place. This is just one of the many reasons why I recommend taking a high quality omega-3 supplement in the form of krill oil, which I have found to be the most effective and beneficial, compared to fish oil. |
|
Related Articles:
 Major Confusion on How to Do Breast Checks
Major Confusion on How to Do Breast Checks
 Your Immune System Can Keep Cancer Dormant
Your Immune System Can Keep Cancer Dormant
 How You Can Beat Prostate and Breast Cancer Nutritionally
How You Can Beat Prostate and Breast Cancer Nutritionally