Fiber Provides Food to Your Gut Microbes That They Ferment to Shape Your DNA
Dr. Mercola
Your body is a complex ecosystem made up of more than 100 trillion bacteria, fungi, viruses, and protozoa, collectively referred to as your microbiome, which must be properly balanced and cared for if you want to maintain good health.
These microbes are so numerous they actually outnumber the cells in your body 10 to one. With such a high prevalence of microbes in your system, it seems reasonable to suspect that they're of some major importance.
And indeed, recent years have brought a scientific flurry of information demonstrating just how crucial your microbiome is to everything from genetic expression, immune function, body weight and composition, to mental health, memory, and the prevention of numerous diseases, from diabetes to cancer.
For example, in one study,1 DNA analysis of diseased sections of intestine removed from patients suffering from Crohn's disease revealed that one particular bacterium, Faecalibacterium prausnitzii, was lower than normal.
While researchers have linked the overabundance of specific bacteria to various diseases, this finding suggests certain anti-inflammatory microbes may be actively involved in preventing certain disease states and when they're lacking, you end up losing this protection.
Recent research also suggests that genes from microbes have become incorporated into human DNA, including some genes that help your immune system defend itself against infections.
Modern Diseases Linked to Alterations in Intestinal Microflora
The composition of the human microbiome varies from person to person based on factors such as diet, health history, geographic location, and even ancestry, and it's readily influenced by diet, chemical exposures, hygiene, and other environmental factors.
In fact, it's become increasingly clear that destroying your gut flora with antibiotics and pharmaceutical drugs, harsh environmental chemicals, and toxic foods is a primary factor in rising disease rates.
The reason for this is because your gut is actually the proverbial gatekeeper for your inflammatory response, and inflammation tends to be a hallmark of most chronic diseases.
The inflammatory response starts in your gut and then travels to your brain, which subsequently sends signals to the rest of your body in a complex feedback loop. It isn't important that you understand all of the physiology here, but the take-away message is that your gut flora's influence is far from local. It significantly affects and controls the health of your entire body.
Microbial Genes Are Passed from Parent to Child
It's important to realize that the foundation of a person'sgut flora is laid from birth. Just like other genetic information, microbes (and their genetic material) are passed on from parent to child.
A baby basically "inherits" the microbiome from its mother as it passes through the birth canal (provided it's a vaginal birth). This is why it's so important to address your gut health before, during, and after pregnancy.
Microbes are also passed between mother and child via breast milk and close body contact in general. As noted in a recent article by Scientific American,2 all of these transfers are crucial for the child's health, but can easily be circumvented by medical interventions and modern "conveniences":
"Because the critical issue is the intergenerational transfer of microbes and its timed assembly, three periods are relevant: before pregnancy, during pregnancy and in the child's early life.
For all three periods, antibiotic use is relevant because it may directly change maternal microbes prior to transfer or the child's microbes afterward.
Elective cesarean sections mean that the child misses the birth canal transit, and antibacterials in soaps and foods directly affect microbiota composition.
Infant formulas have not been constructed with the benefit of millions of years of mammalian evolution, because breast milk contains nutrients that specifically select for the growth of preferred coevolved organisms and inhibit opportunists and pathogens."
Unfriendly (or lacking) flora can predispose babies to Gut and Psychology Syndrome (GAPS), which can raise the child's risk of any number of health problems, including autism and autoimmune disorders.
Babies who develop abnormal gut flora are left with compromised immune systems, which may turn out to be a crucial factor when it comes to vaccine-induced damage.
As explained by Dr. Campbell-McBride, vaccinations were originally developed for children with healthy immune systems, and children with abnormal gut flora and therefore compromised immunity are not suitable candidates for our current vaccine schedule as they're more prone to being harmed. To learn more about this, please see this previous article.
Microbe Genes Found in Human DNA
Some of the latest research3 in this arena reveals that bacteria, fungi, and viruses may be part of the "missing link" in the progress of humans. As noted in a report by CNN:4
"Though most of our genes come from primate ancestors, many of them slipped into our DNA from microbes living in our bodies, says British researcher Alastair Crisp. It's called horizontal gene transfer...
Bacteria slip genes to each other, and it helps them evolve. And scientists have seen insects pick up bacterial genes that allow them to digest certain foods... Humans may have as many as hundreds of so-called foreign genes they picked up from microbes."
The human genome consists of about 23,000 genes, whereas the combined genetic material of your microbiome is somewhere between 2-20 million. According to the researchers, these extra genes may have played a role in helping to diversify our own DNA.
In this study,5 researchers at the University of Cambridge identified 128 "foreign" genes in the human genome, including the gene that determines your blood type (A, B, or O). This gene, and others—including some that help your immune system defend itself against infections—appear to have been transferred into the human gene pool from microbes.
Microbes That Ferment Fiber Are Important for Health
One of the quickest and easiest ways to improve your gut health is via your diet, as the microbes in your body consume the same foods you do. The beneficial ones tend to feed on foods that are known to benefit health, and vice versa. Sugar, for example, is a preferred food source for fungi that produce yeast infections and sinusitis, whereas healthy probiotic-rich foods like fermented vegetables boost populations of health-promoting bacteria, thereby disallowing potentially pathogenic colonies from taking over.
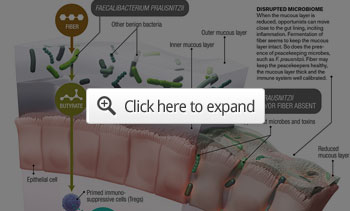
Fiber is also important for a healthy microbiome. Some of the microbes in your gut specialize in fermenting soluble fiber found in legumes, fruits, and vegetables, and the byproducts of this fermenting activity help nourish the cells lining your colon. Some of these fermentation byproducts also help calibrate your immune system, thereby preventing inflammatory disorders such as asthma and Crohn's disease.6,7
Source: Illustration by AXS Biomedical Animation Studio; Source: "Feed Your Tregs More Fiber," by Julia Bollrath and Fiona Powrie, In Science, Vol. 341; August 2, 2013.8
Your intestine harbors over 500 different species of microbes, and research suggests virtually all of these have the ability to affect your health in one way or another, although we still do not fully understand all the mechanisms and pathways by which they do so. It is a quickly evolving field however, and we're learning more with each passing year. For example, research published a couple of years ago show that common bacterial metabolites—short-chain fatty acids (SCFAs)—selectively expand regulatory T cells called Tregs, which are critical for regulating intestinal inflammation.9
According to one of these studies:10 "Treg cells suppress the responses of other immune cells, including those that promote inflammation. This finding provides a new link between bacterial products and a major anti-inflammatory pathway in the gut." Other research11,12 has linked Tregs—which are fed by dietary fiber—to the prevention and reversal of metabolic syndrome, in part by stimulating oxidative metabolism in your liver and adipose tissue.
Are You Getting Enough High-Quality Fiber?
Dietary guidelines call for 20-30 grams of fiber per day. I believe an ideal amount for most adults is around 32 grams daily. Most people, however, get only half that, or less. Many whole foods, especially fruits and vegetables, naturally contain bothsoluble and insoluble fiber. This is ideal, as both help feed the microorganisms living in your gut. The same cannot be said for grains (including whole grains) and processed foods, as the carbohydrates found in both can serve as fodder for microorganisms that tend to be detrimental rather than beneficial to your health.
Gliadin and lectins in grains may also increase intestinal permeability or leaky gut syndrome. So, to maximize your health benefits, focus on eating more vegetables, nuts, and seeds. The following is a small sampling of foods that contain high levels of soluble and insoluble fiber.
Psyllium seed husk, flax, and chia seeds Berries Vegetables such as broccoli and Brussels sprouts Root vegetables and tubers, including onions, sweet potatoes, and jicama Almonds Peas Green beans Cauliflower Beans A simple tip to increase the amount of fiber and biodense nutrients in your diet would be to add sunflower sprouts to your meal. They work great in salads but can also be added to virtually any dish to radically improve its nutrition. Organic whole husk psyllium is another effective option. Taking it three times a day could add as much as 18 grams of dietary fiber (soluble and insoluble) to your diet. Opting for an organic version of psyllium will prevent exposure to pesticides, herbicides, and chemical fertilizers, as conventional psyllium is a very heavily sprayed crop. I also recommend choosing one that does not contain additives or sweeteners, as these tend to have a detrimental effect on your microbiome.
Optimizing Your Microbiome May Be One of Your Most Important Disease Prevention Strategies
Optimizing your gut flora may be one of the most important things you can do for your health, and the good news is that this isn't very difficult. However, you do need to take proactive steps. To optimize your microbiome both inside and out, consider the following recommendations:
| Do | Avoid |
|---|---|
| Eat plenty of fermented foods.Healthy choices include lassi, fermented grass-fed organic milk such as kefir, natto (fermented soy), and fermented vegetables. If you ferment your own, consider using a special starter culture that has been optimized with bacterial strains that produce high levels of vitamin K2. This is an inexpensive way to optimize your K2, which is particularly important if you're taking a vitamin D3 supplement. | Antibiotics, unless absolutely necessary (and when you do, make sure to reseed your gut with fermented foods and/or a probiotic supplement). And while some researchers are looking into methods that might help ameliorate the destruction of beneficial bacteria by antibiotics,13,14 your best bet is likely always going to be reseeding your gut with probiotics from fermented and cultured foods and/or a high-quality probiotic supplement. |
| Take a probiotic supplement. Although I'm not a major proponent of taking many supplements (as I believe the majority of your nutrients need to come from food), probiotics is an exception if you don't eat fermented foods on a regular basis | Conventionally raised meats and other animal products, as CAFO animals are routinely fed low-dose antibiotics, plus genetically engineered grains, which have also been implicated in the destruction of gut flora. |
| Boost your soluble and insoluble fiber intake, focusing on vegetables, nuts, and seeds, including sprouted seeds. | Chlorinated and/or fluoridated water. |
| Get your hands dirty in the garden. Germ-free living may not be in your best interest, as the loss of healthy bacteria can have wide-ranging influence on your mental, emotional, and physical health. According to the hygiene hypothesis, exposure to bacteria and viruses can serve as "natural vaccines" that strengthen your immune system and provide long-lasting immunity against disease. Getting your hands dirty in the garden can help reacquaint your immune system with beneficial microorganisms on the plants and in the soil. |
Processed foods. Excessive sugars, along with otherwise "dead" nutrients, feed pathogenic bacteria. Food emulsifiers such as polysorbate 80, lecithin, carrageenan, polyglycerols, and xanthan gum also appear to have an adverse effect on your gut flora.15
Unless 100% organic, they may also contain GMOs that tend to be heavily contaminated with pesticides such as glyphosate. |
| Open your windows. For the vast majority of human history the outside was always part of the inside, and at no moment during our day were we ever really separated from nature. Today, we spend 90 percent of our lives indoors. And, although keeping the outside out does have its advantages it has also changed the microbiome of your home. Research16 shows that opening a window and increasing natural airflow can improve the diversity and health of the microbes in your home, which in turn benefit you. | Agricultural chemicals, glyphosate (Roundup) in particular. |
| Wash your dishes by hand instead of in the dishwasher. Recent research has shown that washing your dishes by hand leaves more bacteria on the dishes than dishwashers do, and that eating off these less-than-sterile dishes may actually decrease your risk of allergies by stimulating your immune system. | Antibacterial soap, as they too kill off both good and bad bacteria, and contribute to the development of antibiotic-resistance. |
SEE VIDEO
http://articles.mercola.com/sites/articles/archive/2015/03/30/fiber-fermentation-gut-health.aspx