
A Comprehensive Guide to Glaucoma
Paige Watts
In the UK, it is estimated that 300,000 people are unknowingly living with glaucoma. In this guide, we’ll explore the importance of understanding glaucoma, what its symptoms are and how it can be treated. We’ll also look at some of the most frequently asked questions about this eye condition, including what the different types of glaucoma are.
What Is Glaucoma?
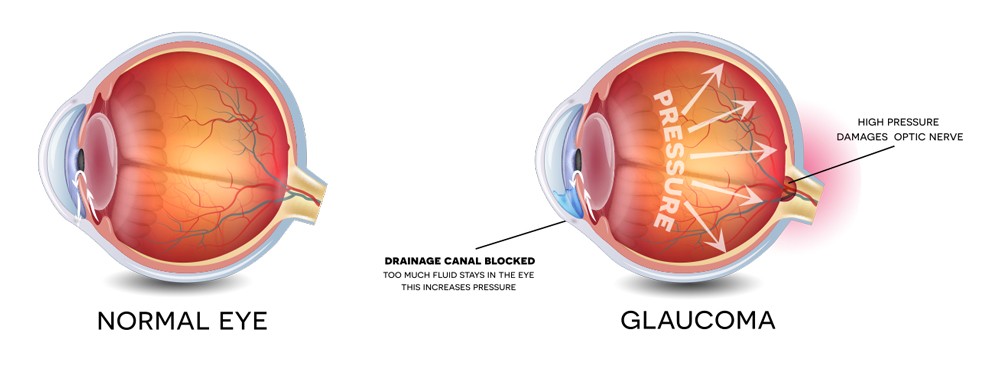
Glaucoma is a condition that damages your optic nerve, which is the part of your eye that’s connected to the brain. If it isn’t detected and treated in its early stages, it can lead to vision loss.
Glaucoma normally arises when the fluid in your eye isn’t able to drain away properly. This increases the pressure inside your eye, which subsequently puts pressure on your optic nerve.
 Due to the fact glaucoma doesn’t always have telltale symptoms in its early stages, people can be suffering from the condition without realising it. Despite this, it is a common condition and affects all age groups, including young children and babies. It is most common in people aged 70+.
Due to the fact glaucoma doesn’t always have telltale symptoms in its early stages, people can be suffering from the condition without realising it. Despite this, it is a common condition and affects all age groups, including young children and babies. It is most common in people aged 70+.
The Types of Glaucoma and Their Symptoms
Glaucoma comes in several different types, and each of these has different causes, symptoms and treatments. The main types are:
Primary Open-Angle Glaucoma
This is the most common type of glaucoma, and can also be referred to as chronic open-angle glaucoma.
This type of glaucoma means the fluid in your eye doesn’t drain properly, but the angle (the part of your eye where the fluid is drained) isn’t blocked. However, because the fluid isn’t draining properly, it still adds pressure to your eye.
Usually, there won’t be any significant symptoms at the start and it will typically develop slowly over a number of years. And because the peripheral vision is the first thing that’s affected, people are often unaware they’ve developed the condition. Nevertheless, without the right treatment, vision in the centre of the eye can also be lost.
Primary open-angle glaucoma is normally detected in a routine eye examination, which is recommended every two years (at least). If you are concerned about any changes in your vision, you should visit your local optician.
Primary Angle-Closure Glaucoma
This type of glaucoma is less common, and means the angle of your eye, where the fluid drains away, becomes blocked, which increases the pressure in your eye.
Even though primary angle-closure glaucoma develops slowly over time, it can often cause sudden symptoms that are quite severe. These include headaches, a red eye, intense eye pain, blurred vision, seeing halos around lights, tenderness to the area around the eye and feeling or being sick.
These symptoms can last for a couple of hours before disappearing. However, if you do notice any of these symptoms, you should visit your nearest A&E department or eye casualty unit as soon as possible.
Secondary Glaucoma
Caused by another eye issue, secondary glaucoma is an uncommon form of glaucoma. The causes include certain treatments (e.g. operations or medication), eye injuries and uveitis (where the middle layer of your eye becomes inflamed).
Symptoms do vary significantly between each patient but can include a red eye, eye pain, halos around lights, blurred vision and a gradual loss of your peripheral vision. Again, if you are concerned about any noticeable changes in your vision, visit your optician straight away, or A&E if you feel your symptoms are severe and have occurred suddenly.
Congenital Glaucoma
Also known as developmental glaucoma or childhood glaucoma, this type affects young children and babies.
It usually stems from a problem in how their eyes are developing, which causes the fluid and pressure in their eye to start building.
Often, it can be difficult to spot this condition in your child, but some symptoms to look out for include frequent rubbing of the eyes; cloudy, watery or red eyes; uncontrollable blinking; a dislike of bright lights and larger-than-usual eyes.
If you do notice any of these symptoms in your child’s eye(s), visit your GP or optician immediately.
What Causes Glaucoma?
In most cases, glaucoma is caused by pressure building up in your eye, but there are a number of other reasons why it might occur.
Inside the eye is aqueous humour, which is a watery substance that gives your eye its shape by creating pressure within it. This fluid is constantly flowing in and out of the eyes when they’re healthy.
However, if this fluid cannot drain away properly, pressure can start to build, which damages the optic nerve (the part of the eye that sends signals to your brain).
Why this happens is often unclear, but there are a few known causes:
- Previous eye surgery or an eye injury
- The use of steroid eye drops over a long period of time
- Uveitis – when the middle layer of your eye gets inflamed
- Blocked drainage due to new blood vessels that grow in your eye
- Deposit build-up in the eye’s drainage tubes – causing conditions like pseudoexfoliation glaucoma
- Problems that arise while the eyes are developing, which can cause glaucoma in young children and babies
There are also some factors that increase your risk of developing glaucoma.
What Increases Your Risk Of Developing Glaucoma?
There are several factors that can increase your risk of developing this eye condition, including:
1. Age
As you get older, the chances of you developing glaucoma become more likely. 2% of those aged 40 and over, and 10% of those aged 75 and over are affected by primary open-angle glaucoma (the most common type).
2. Ethnic Origin
Certain types of glaucoma are more likely to develop in people of Asian, Afro-Caribbean and African origin.
3. Family History
You’re at an increased risk of developing glaucoma if a close member of your family has it too – i.e. your mum or dad, or your brother or sister.
4. Other Medical Conditions
Your risk of glaucoma can also be increased by other conditions such as diabetes, long sightedness and short-sightedness.
How Is Glaucoma Diagnosed?
Before glaucoma causes any symptoms, it’s usually picked up in a routine eye test, which is why having regular tests is so important. By detecting glaucoma early, it can prevent your vision from deteriorating significantly.
It’s recommended to have an eye test around every two years, but if you’re at high risk of developing glaucoma, you might be told to have these tests on a more frequent basis.
Glaucoma Tests
To diagnose glaucoma and to continually monitor it, there are a number of pain-free, quick tests that can be conducted.
Eye Pressure Test (Tonometry)
This test involves using a tonometer to measure your eye’s pressure. To do this, a small amount of dye and anaesthetic is placed into your eye. The tonometer is then held gently up to your eye and its light helps measure the inner pressure of your eye.
If the test reveals high pressure, it could indicate that you’re at risk of developing glaucoma or have already got it.
Gonioscopy
During this test, the outer edge of your eye is examined – this is the bit between your iris (the part of your eye that’s coloured) and the cornea (the transparent layer that covers your eye at the front).
It is in this area where the fluid of your eye should drain away. The gonioscopy will establish whether the angle (the area in question) is closed or open, which could be affecting how fluid is draining out of your eye.
Visual Field Test
Sometimes called perimetry, a visual field test will check to see whether there are any areas of vision that are missing.
To conduct this test, you may be asked to look at a sequence of light spots, indicating when you can see one. Some dots will appear in the side of your vision (your peripheral vision) – this is the area that’s often affected during the early stages of glaucoma.
If you aren’t seeing the lights that are appearing in this area, it could indicate that your vision has been damaged by glaucoma.
Optic Nerve Assessment
In glaucoma, the nerve that connects your eye and brain, the optic nerve, can be damaged, so it may be necessary to assess this nerve to see if it’s still healthy.
To carry out this test your pupils need to be enlarged, so a few eye drops will be placed into your eyes to do this. A slit lamp (a microscope that emits a bright light) will be used to examine your eyes and optic nerve.
As your pupils are widened during this test, it may affect your vision, which is why it’s recommended to take someone with you who can drive you home afterwards.
Optical Coherence Tomography (OCT)
This type of scan produces an image of the back of your eye by using rays of lights to scan it. If any damage has been caused to the retina (the layer at the back of your eye that’s light sensitive) or your optic nerve, the test will help detect this.
When Will You Be Referred to a Glaucoma Specialist?
If during your eye examination, glaucoma is detected, you should be referred for further tests with a specialist eye doctor (an ophthalmologist).
During these further tests, your ophthalmologist will be able to establish how far developed the condition is, how much damage has been caused by glaucoma and what the potential causes of this condition are.
After this, they will be able to advise what treatments should be undertaken. Sometimes, these treatment options will be provided by your ophthalmologist, but if your case isn’t of a serious nature, you may be referred back to your local optician.
How Can Glaucoma Be Treated?
There are a number of different ways glaucoma can be treated, with each treatment depending on a patient’s circumstances and the severity of the condition.
Even though these treatments can’t reverse any vision loss that’s already occurred, it can help prevent your vision from becoming any worse.
What Treatment Plans are Available for the Different Types of Glaucoma?
The type of glaucoma you have will often influence the treatment you receive, for example:
Treatment for Primary Open-Angle Glaucoma
This is often treated using eye drops, or, if these don’t help, surgery or laser treatment may be recommended.
Treatment for Primary Angle-Closure Glaucoma
Due to the nature of this type of glaucoma, immediate treatment is often required. This involves a hospital visit where medication is used to try and reduce the eye’s pressure. Laser treatment will often follow this.
Secondary Glaucoma
Depending on what’s caused this glaucoma, eye drops, surgery or laser treatment may be used to treat it.
Congenital Glaucoma
As this is often caused by another problem in the eye which has caused pressure and fluid to build up, surgery is often needed to correct this issue first.
After your treatment, you will have regular appointments that help your ophthalmologist to see whether the treatment has been effective.
Using Eye Drops to Treat Glaucoma
The main type of treatment for this eye condition is eye drops, and even though there are many different types of these, they all work to reduce how much pressure there is in your eyes. Some of the most commonly used eye drops include:
- Prostaglandin Analogues – g. Travoprost, Tafluprost, Bimatoprost and Latanoprost
- Miotics: g. Pilocarpine
- Carbonic Anhydrase Inhibitors: g. Dorzolamide and Brinzolamide
- Beta-Blockers: g. Timolol, Levobunolol Hydrochloride and Betaxolol Hydrochloride
- Sympathomimetics: g. Brimonidine Tartrate
Some of the side effects of these eye drops include irritation, and certain ones won’t be suitable if you’re suffering from other underlying conditions.
To find the most effective one for you, you may need to try a few different types first. And some people need to use more than one of these eye drops at the same time.
How to Use Eye Drops Effectively
These prescribed eye drops will normally be used up to four times a day, and it’s crucial you use them as you’ve been directed. Even if you haven’t noticed any issues with your eyesight, it’s still important to use these drops as your sight could be at risk if not.
To correctly apply the eye drops to your eye, simply pull down your lower eyelid with your finger. Hover the eye drops over your eye and squeeze the bottle to release a drop into the pocket you’ve created by pulling out your lower lid. Then, close your eye for a few minutes.
If you are using more than one eye drop, make sure you allow five minutes between each application.
Using Laser Treatment for Glaucoma
Laser treatment may be required if your symptoms haven’t improved when using eye drops.
This treatment involves a beam of high-energy light being directed at your eye to try and stop fluid and pressure from building up. These types of treatments include:
- Laser Trabeculoplasty: To open up your eye’s drainage tubes, a laser is used. This allows more of the fluid in your eye to drain out, reducing the pressure inside it.
- Laser Iridotomy: Holes in your iris are made using a laser, allowing fluid to drain out of your eye.
- Cyclodiode Laser Treatment: This laser destroys some of your eye’s tissue that produces the liquid in your eye (aqueous humour), which can help remove some of the pressure in your eye.
These procedures tend to be performed while you’re awake, with local anaesthetic drops being used to numb the eye. During the operation, you may experience some heat and brief twinges of pain. After the treatment, you may need to carry on using eye drops.
Using Surgery to Treat Glaucoma
In some cases, surgery will be recommended instead of laser treatment. There are a number of different types of surgery for glaucoma, including:
- Trabeculectomy: This is the most common operation for glaucoma and helps fluid drain out of your eye more easily by removing part of the drainage tubes that are preventing this.
- Trabeculotomy: This procedure is very similar to the above but a small part of the eye is removed using an electric current instead.
- Deep Sclerectomy: An operation that widens the eye’s drainage tubes to provide better flow of the eye’s fluid. Sometimes, this involves placing a tiny device inside your eye.
- Viscocanalostomy: Part of the sclera (the white outer that covers your eyeball) is removed in this operation, helping the eye’s fluid to drain more easily
- Trabecular Stent Bypass: To increase the fluid drainage in your eye, a tiny tube is placed within your eye in this operation.
These types of surgeries can be carried out while you’re asleep (using general anaesthetic) or they may be carried out while you’re awake (using local anaesthetic).
http://www.lasereyesurgeryhub.co.uk/a-comprehensive-guide-to-glaucoma/
