WHEN HOSPITALS BUY DOCTORS' OFFICES, AND PATIENT FEES SOAR
Margor Sanger-Katz
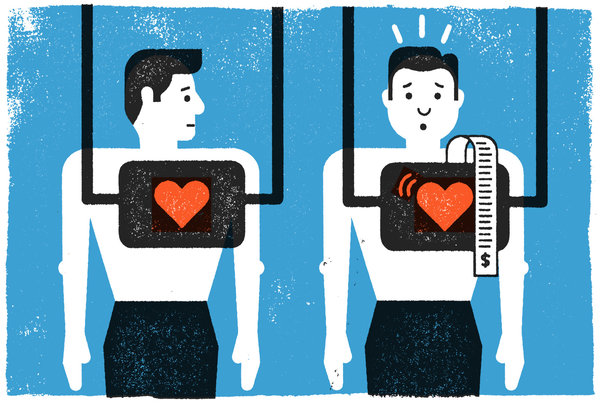
Imagine you’re a Medicare patient, and you go to your doctor for an ultrasound of your heart one month. Medicare pays your doctor’s office $189, and you pay about 20 percent of that bill as a co-payment.
Then, the next month, your doctor’s practice has been bought by the local hospital. You go to the same building and get the same test from the same doctor, but suddenly the price has shot up to $453, as has your share of the bill.
Patients around the country are getting that unpleasant surprise, as more and more doctors’ offices are being bought by hospitals. Medicare, the government health insurance program for those 65 and over or the disabled, pays one price to independent doctors and another to doctors who work for large health systems — even if they are performing the exact same service in the exact same place.
This week, the Obama administration recommended a change to eliminate much of that gap. Despite expected protests from hospitals and doctors, the idea has a chance of being adopted because it would yield huge savings for Medicare and patients.
In the dry language of the annual budget, the White House asks Congress to “encourage efficient care by improving incentives to provide care in the most appropriate ambulatory setting.” In normal English, that means reducing financial incentives that are causing many doctors to sell their practices to hospitals just to take advantage of extra revenue.
The heart doctors are a great example. In 2009, the federal government cut back on what it paid to cardiologists in private practice who offered certain tests to their patients. Medicare determined that the tests, which made up about 30 percent of a typical cardiologist’s revenue, cost more than was justified, and there was evidence that some doctors were overusing them. Suddenly, Medicare paid about a third less than it had before.
But the government didn’t cut what it paid cardiologists who worked for a hospital and provided the same test. It actually paid those doctors more, because the payment systems were completely separate. In general, Medicare assumes that hospital care is by definition more expensive to provide than office-based care.
You can imagine the result: Over the past five years, the number of cardiologists in private practice has plummeted as more and more doctors sold their practices to nearby hospitals that weren’t subject to the new cuts. Between 2007 and 2012, the number of cardiologists working for hospitals more than tripled, according to a survey from the American College of Cardiology, while the percentage working in private practice fell to 36 percent from 59 percent. At the time of the survey, an additional 31 percent of practices were either in the midst of merger talks or considering it. The group’s former chief operating officer once described the shift to me as “like a migration of wildebeests.”
Cardiologists are not the only doctors who have been migrating toward hospital practice. In the last few years, there have been increases in the number of doctors working for hospitals across the specialties. And spreads between fees for office services exist in an array of medical services, down to the basic office visit. The president's proposal would apply to all doctors working in off-campus, hospital-owned practices.
Shifting practice ownership patterns have ripple effects for patients with private insurance, too. Like Medicare, most private insurers pay higher prices to hospitals than to independent doctors.
Private insurers tend to copy many of Medicare’s payment policies. And, in general, large hospital groups tend to have more negotiating clout with insurers, meaning they can bargain for higher prices than smaller practices.
The administration’s proposal would essentially end that system of different prices for similar services. Medicare would pay the same for any visit, test or procedure offered by doctors who work in private practice and by those who work in off-campus practices that are owned by hospitals. Doctors who work in the hospital building could still be paid the higher hospital rate. But the free-standing practice that suddenly changes hands would not continue to be paid more.
The result, in dollar terms, is estimated to be very large. According to the White House’s calculation, Medicare would save nearly $30 billion over 10 years if Congress required the payment switch. That’s more than Medicare could save if it raised the eligibility age to 67. And that doesn’t even count the money that could be saved by Medicare patients whose co-payments will also go down.
Hospitals don’t like the idea. Nearly all the money would come out of their pockets, and they argue that running a medical practice really does cost more for hospitals than it does for independent physician practices. Hospitals have to stay open at all hours, run emergency rooms and comply with an array of regulatory requirements that physician-owned practices don't need to worry about.
“You can't just convert it and be exactly the same,” said Rich Pollack, an executive vice president at the American Hospital Association. “You have to meet the requirements.”
The Medicare Payment Advisory Committee, a group of experts that advises Congress, thinks that the pay differences should be narrowed, but only for a select set of medical services in which it’s really clear that there’s no difference between the care offered by a hospital and a physician office.
The pay differences, of course, are not the only reason that more doctors are going to work for hospitals. There are generational trends: Younger doctors are less interested in entrepreneurship and more interested in predictable hours and salary. And another Medicare program is trying to create financial incentives for health systems to manage patients’ entire health care experience, which many hospitals find easier to do if they employ the doctors.
Still, Robert Berenson, a physician and a senior fellow at the Urban Institute, said it’s clear that a lot of recent doctor-hospital mergers have been driven by Medicare’s disparate pay policies. He thinks the budget proposal lacks needed subtlety, but he supports equalizing many payments in concept. “If hospitals are going to employ physicians, it should be done for the right reasons, not the wrong reasons,” he said.
The change would have big consequences, especially for hospitals, which have already endured several rounds of recent Medicare cuts. But in contrast to a lot of things in the president’s budget, it’s hard to dismiss this proposal as mere wishful thinking. Congress is often looking for places to save money in the Medicare budget, in part because it must find money every year to keep all doctors’ pay from declining precipitously — the result of a misguided payment formula passed in the 1990s.
“The list of available offsets is dwindling,” said Eric Zimmerman, a partner at the lobbying firm McDermott Will & Emery, who represents many health care providers. In an email, he described the doctor’s pay proposal as one that “may be moving to the top of the list.”
http://www.nytimes.com/2015/02/07/upshot/medicare-proposal-would-even-out-doctors-pay.html