
Fraud Case Rocks Anesthesiology Community
Adam Marcus
In what experts are calling one of the largest known cases of academic misconduct, a leading anesthesiology researcher has been accused of falsifying data and other fraud in potentially dozens of published studies.
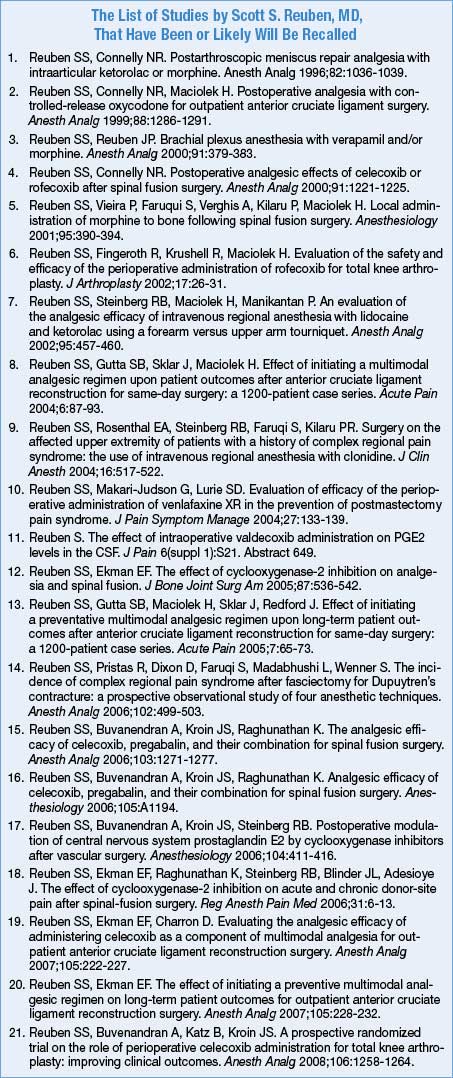
Scott S. Reuben, MD, of Baystate Medical Center in Springfield, Mass., a pioneer in the area of multimodal analgesia, is said to have fabricated his results in at least 21, and perhaps many more, articles dating back to 1996. The confirmed articles were published in Anesthesiology, Anesthesia and Analgesia, the Journal of Clinical Anesthesia and other titles, which have retracted the papers or will soon do so, according to people familiar with the scandal (see list). The journals stressed that Dr. Reuben’s co-authors on those papers have not been accused of wrongdoing.
In addition to allegedly falsifying data, Dr. Reuben seems to have committed publishing forgery. Evan Ekman, MD, an orthopedic surgeon in Columbia, S.C., said his name appeared as a co-author on at least two of the retracted papers, despite his having had no hand in the manuscripts. “My names were forgeries on the documents,” Dr. Ekman told Anesthesiology News.
Dr. Reuben has been an extremely active and visible figure in multimodal analgesia, particularly as an advocate for its use in minimally invasive orthopedic and spine procedures. His research has provided support for several mainstays of current anesthetic practice, such as the use of nonsteroidal anti-inflammatory drugs and neuropathic agents instead of opioids and preemptive analgesia. Dr. Reuben has also published and presented data suggesting that multimodal analgesia can significantly improve long-term outcomes for patients.
Incomprehensible Course
All of that is now in question, said Steven L. Shafer, MD, editor-in-chief of Anesthesia and Analgesia, which retracted 10 of Dr. Reuben’s articles. “We are left with a large hole in our understanding of this field. There are substantial tendrils from this body of work that reach throughout the discipline of postoperative pain management,” Dr. Shafer said. “Those tendrils mean that almost every aspect will need to be carefully thought through. What do we still believe to be true? Do the conclusions hold up to scrutiny?”
Dr. Shafer said that although he still believes “philosophically” in multimodal analgesia, he can no longer be absolutely certain of its benefits without confirmation from future studies.
Dr. Shafer called the scandal “a tragedy” for the profession, for patients and for Dr. Reuben personally. “I cannot begin to comprehend why a person would take this course,” he said of the research fraud.
Efforts to reach Dr. Reuben were unsuccessful.
Internal Inquiry Revealed Sweeping Misconduct
The retractions came after an internal investigation by Baystate turned up evidence of widespread fraud in Dr. Reuben’s research. Jane Albert, a spokeswoman for Baystate, said the inquiry was undertaken after an internal reviewer at the medical center had raised questions last year. Ms. Albert said the hospital’s investigation raised “no allegations concerning any patient care. This was focused on academic integrity.”
Dr. Reuben is on medical leave from his position as chief of the acute pain service at Baystate, Ms. Albert said.
 Dr. Reuben, who was educated at Columbia University and received his medical degree from SUNY at Buffalo School of Medicine, is well-known among anesthesiology researchers for his studies of multimodal analgesia, the practice of combining several forms of pain relief to better control postoperative discomfort and promote faster recovery from surgery.
Dr. Reuben, who was educated at Columbia University and received his medical degree from SUNY at Buffalo School of Medicine, is well-known among anesthesiology researchers for his studies of multimodal analgesia, the practice of combining several forms of pain relief to better control postoperative discomfort and promote faster recovery from surgery.
Rumors of a problem with Dr. Reuben’s research have been circulating among academic anesthesiologists for a year, according to people familiar with the matter.
"Interestingly, when you look at Scott’s output over the last 15 years, he never had a negative study,” said one colleague, who spoke on the condition of anonymity. “In fact, they were all very robust results—where others had failed to show much difference. I just don’t understand why anyone would do this or how anyone could pull this off for so long.”
A recent PubMed search for Dr. Reuben’s name turned up 72 citations, the most recent an article in the December issue of the Journal of Cardiothoracic and Vascular Anesthesia on preventing the development of chronic pain after thoracic surgery.
“Massive” Breach of Trust
Josephine Johnston, an attorney specializing in research integrity at the Hastings Center, in Garrison, N.Y., called the scope of the Reuben fraud “massive.”
"It’s usually just one article, not a body of work,” Ms. Johnston said.
What’s particularly surprising given the dimensions of the case, Ms. Johnston said, is that Dr. Reuben’s research managed to raise no alarms among peer reviewers. However, she added, “the peer review system can only do so much. Trust is a major component of the academic world. It’s backed up by the implication that your reputation will be destroyed if you violate that trust.”
A cornerstone of Dr. Reuben’s approach has been the use of the selective cyclooxygenase-2 inhibitor celecoxib (Celebrex) and the neuropathic pain agent pregabalin (Lyrica), both manufactured by Pfizer. Dr. Reuben has received research grants from the company and is a member of its speakers’ bureau. However, a source told Anesthesiology News that Pfizer recently alerted its speakers to remove any reference to Dr. Reuben’s data from their presentations. Pfizer was unable to comment by the time this article went to press. The company has not been accused of wrongdoing in the matter.
Jacques Chelly, MD, PhD, MBA, director of the Division of Regional Anesthesia and Acute Interventional Perioperative Pain at the University of Pittsburgh Medical Center (UPMC), said that the Reuben episode has left multimodal analgesia “in shambles concerning many of the drugs we use”—particularly celecoxib and pregabalin. “The big chunk of what people have based their protocol on is gone.”
In light of the situation and economic concerns, UPMC has stopped giving celecoxib and pregabalin to surgery patients “until we have some very formal evidence that we should do something else,” Dr. Chelly said. “In this day and age, doing multimodal [therapy] is expensive. Any institution is going to look at evidence-based clinical decisions, and unless we have very strong data, it is a problem.”
One of the pillars of support for combining celecoxib and pregabalin was a 2006 study in Anesthesia and Analgesia—for which Dr. Reuben has been a reviewer—by Dr. Reuben and colleagues that found the approach effective in patients undergoing spinal surgery. That paper has been withdrawn. “If we take out [those] data in spinal,” Dr. Chelly said, “you really don’t have any evidence that the combination is working.”
(March, 2009)
Feb. 20, 2010
www.anesthesiologynews.com/index.asp
